Hemoglobinuria: Unexpected Signals You Must Not Ignore
Hemoglobinuria is a rare but serious condition that may silently signal underlying health issues. While often unnoticed in early stages, certain unexpected symptoms could point to a more significant problem. Understanding these signs is essential for timely diagnosis and treatment. This article uncovers the key warning signals of hemoglobinuria and what they could mean for your health.
Urine that turns tea-colored, cola-colored, or unusually dark can be alarming, and for good reason. One important cause is hemoglobinuria, which happens when hemoglobin (the oxygen-carrying protein inside red blood cells) appears in urine. Because this finding can be linked to significant blood or muscle breakdown, it’s worth treating as a meaningful clue rather than a cosmetic change.
What is Hemoglobinuria?
Hemoglobinuria means free hemoglobin is present in the urine, usually because red blood cells have broken apart in the bloodstream (intravascular hemolysis). The kidneys filter the released hemoglobin, which can darken urine. This differs from hematuria, where intact red blood cells are present in urine due to bleeding somewhere in the urinary tract (for example, a kidney stone).
A practical detail often used in clinics: a urine dipstick may read “blood” in both hematuria and hemoglobinuria. Microscopy helps separate them—hemoglobinuria often shows a positive dipstick with few or no red blood cells seen under the microscope.
What are the Common Causes of Hemoglobinuria?
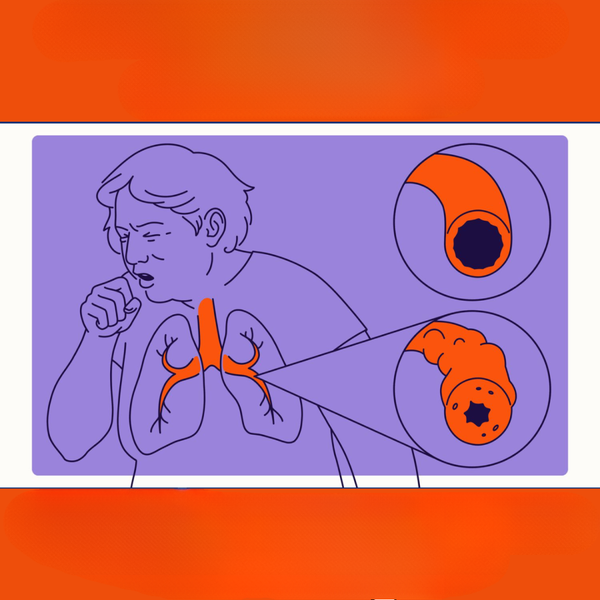
Hemoglobinuria most often points to a process that rapidly damages red blood cells or, less commonly, severe muscle injury (which produces myoglobinuria that can look similar on a dipstick). Clinicians typically think through a short list of categories.
Potential causes include transfusion reactions, certain infections, autoimmune hemolytic anemia, inherited red cell vulnerabilities (such as G6PD deficiency), mechanical hemolysis (for example, from prosthetic heart valves), severe burns, and rare disorders like paroxysmal nocturnal hemoglobinuria (PNH). Intense muscle injury (rhabdomyolysis) can also mimic hemoglobinuria because myoglobin may trigger a similar dipstick result.
What Symptoms Indicate the Presence of Hemoglobinuria?
The urine change itself may be the first noticeable sign, but symptoms often reflect the underlying condition. In intravascular hemolysis, people may experience fatigue, shortness of breath, rapid heart rate, jaundice (yellowing of the skin or eyes), back or abdominal pain, or lightheadedness from anemia. Some report headaches or chest discomfort, depending on severity and individual risk factors.
Urgent warning signs include fainting, severe weakness, confusion, fever with chills (especially after a transfusion), reduced urine output, or swelling—any of which may indicate significant hemolysis, kidney stress, or a serious infection. In PNH specifically, symptoms can also include episodes of dark urine (often more noticeable in the morning), ongoing fatigue, and, in some cases, clotting complications.
How is Hemoglobinuria Diagnosed?
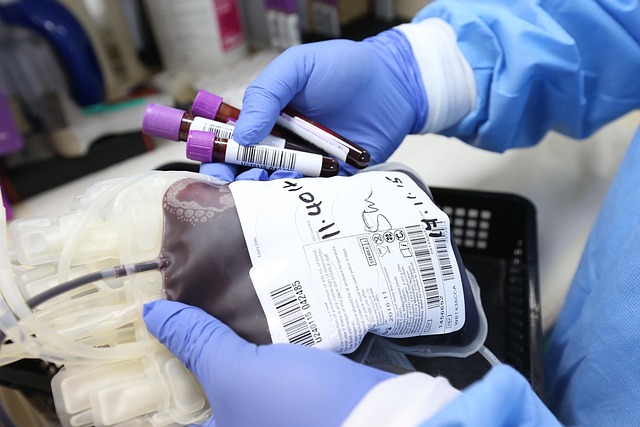
Diagnosis starts with confirming what is actually in the urine. A urinalysis with dipstick and microscopy helps distinguish hemoglobinuria from hematuria. Clinicians may also look for protein levels, urine concentration, and signs of kidney stress. Because myoglobin can resemble hemoglobin on dipstick testing, additional evaluation is often needed when muscle injury is possible.
Blood tests commonly include a complete blood count (to assess anemia), reticulocyte count (bone marrow response), lactate dehydrogenase (LDH), bilirubin, and haptoglobin (often low in intravascular hemolysis). Kidney function tests (creatinine, electrolytes) may be ordered, and creatine kinase (CK) is important when rhabdomyolysis is suspected. If PNH is a concern, flow cytometry testing for specific surface proteins on blood cells is a standard diagnostic approach.
What Treatment Options are Available for Hemoglobinuria?
Treatment depends on the cause, and the initial priority is often preventing complications—especially kidney injury and severe anemia. Hydration may be used in settings where pigment in the urine could harm the kidneys, and clinicians may stop any suspected triggering medication or address an inciting event (such as treating an infection or managing a reaction to a transfusion). If anemia is significant, transfusion or other supportive measures may be considered based on clinical assessment.
When hemoglobinuria is due to hemolytic disorders, care targets the hemolysis itself. For autoimmune hemolytic anemia, treatment may involve immunosuppressive approaches under specialist guidance. If an inherited trigger such as G6PD deficiency is suspected, avoiding oxidative medications and certain exposures can be central to prevention. Mechanical causes (such as valve-related hemolysis) may require cardiology evaluation if persistent.
For PNH, management is typically handled by hematology and may include complement-pathway therapies that reduce intravascular hemolysis and related complications. In the United States, examples of treatments used in appropriate patients include complement inhibitors such as eculizumab and ravulizumab, and other targeted therapies such as pegcetacoplan or iptacopan, depending on individual factors and current clinical guidance. Supportive care can include folate supplementation, iron management (which may be complex in ongoing hemolysis), and careful assessment of clotting risk; anticoagulation decisions are individualized due to benefits and bleeding risks.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.
Recognizing hemoglobinuria as a sign—rather than a diagnosis by itself—helps frame the next steps: confirm whether the urine finding reflects hemoglobin, red blood cells, or muscle pigment; look for evidence of hemolysis or muscle injury in blood tests; and treat the underlying condition while protecting kidney function and overall stability. Prompt evaluation is especially important when symptoms are sudden, severe, or paired with fever, weakness, chest pain, or reduced urination.